In the quest for better sleep, many individuals are exploring the option of at-home sleep studies. The increasing comfort with technology has led to a surge in remote testing opportunities, raising questions about their effectiveness and overall benefits. This article delves into the various aspects of sleep studies, particularly those conducted at home, to help you make informed decisions regarding your sleep health.
Understanding Sleep Studies
Before diving into the specifics of at-home testing, it’s fundamental to grasp what a sleep study entails. Sleep studies, also known as polysomnography, are comprehensive assessments designed to monitor and analyse sleep patterns and phenomena during sleep.
In conclusion, while sleep study at home near me certainly come with their share of advantages, they aren’t without flaws. Weighing these pros and cons carefully will enable you to take the necessary steps towards understanding and improving your sleep health.
What is a sleep study?
A sleep study measures various physiological signals while you sleep, including brain waves, heart rate, breathing patterns, and blood oxygen levels. This diagnostic tool can be conducted in a sleep clinic or the comfort of your own home with appropriate devices.
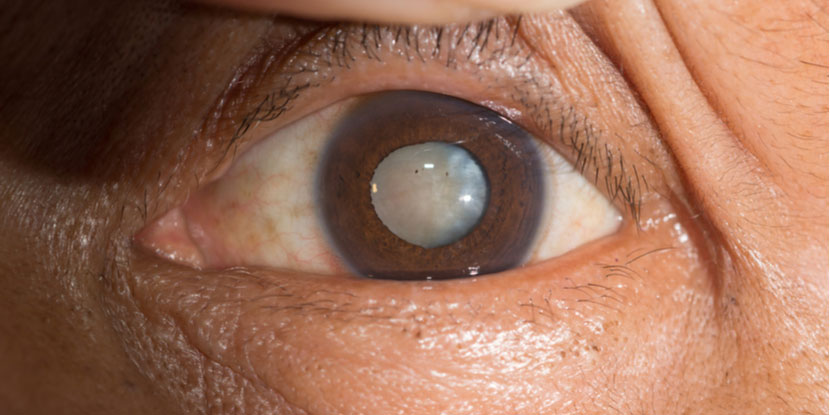
The results from these studies help healthcare professionals diagnose sleep disorders such as sleep apnoea, narcolepsy, and insomnia, leading to targeted treatment plans to enhance sleep quality. In a clinical setting, the study typically involves spending the night in a specially designed room where multiple sensors are attached to monitor your body’s activity. This environment allows for a detailed analysis of sleep stages, including REM (rapid eye movement) and non-REM sleep, which are crucial for restorative sleep.

The importance of diagnosing sleep disorders
Diagnosing sleep disorders is vital for overall health. Untreated conditions can lead to a variety of complications, including daytime fatigue, mood disorders, and even cardiovascular issues. Furthermore, chronic sleep deprivation has been linked to a host of health problems, including obesity, diabetes, and weakened immune function. Recognising the signs of sleep disorders early on can significantly improve not only sleep quality but also overall well-being.
Early detection through reliable sleep studies can lead to effective interventions, helping you reclaim restful nights and revitalised days. In addition to medical treatments, lifestyle changes such as improved sleep hygiene, cognitive behavioural therapy for insomnia (CBT-I), and even dietary adjustments can play a crucial role in managing sleep disorders. Understanding the intricate relationship between sleep and health empowers individuals to take proactive steps towards achieving better sleep, ultimately enhancing their quality of life. Read more about dietary at https://www.canr.msu.edu/news/nutrition_education_and_diet_control
The rise of at-home sleep studies
Advancements in technology and a growing inclination towards convenience have paved the way for at-home sleep studies. These studies allow individuals to monitor their sleep patterns in a familiar and comfortable environment.
How does an at-home sleep study work?
At-home sleep studies typically involve the use of portable devices that you attach to your body before going to bed. These devices monitor various metrics, just like traditional sleep studies done in a clinical setting.
Once you complete the study, the collected data is submitted for analysis. Sleep specialists then interpret the results and provide recommendations based on your sleep patterns.
The convenience of testing in your own home
One of the compelling benefits of at-home testing is the elimination of the need to travel to a medical facility. This is particularly advantageous for individuals who may find it stressful or disruptive to sleep in an unfamiliar environment.
Being in your own home can also lead to more natural sleep patterns, as the usual rituals and comforts of home are maintained throughout the night.
The advantages of at-home sleep studies
At-home sleep studies come with a long list of benefits that appeal to many, from comfort to cost.
Comfort and familiarity
Nothing beats the comfort of your own bed, and that’s a significant factor when it comes to sleep quality. At-home sleep studies offer the chance to rest in a familiar environment, which can lead to more accurate results. Stress often negatively impacts sleep quality, so letting go of the clinical environment can prove beneficial
Cost-effectiveness and time-saving benefits
Traditional sleep studies can be quite costly when you factor in the transportation and time off work. In contrast, at-home studies are generally more affordable and save on travel time. As they are designed to be user-friendly, many individuals find they can conduct the study without professional supervision. To find more about affordable click here.
This cost-effectiveness, coupled with the simplicity of self-monitoring, makes at-home options highly attractive for many consumers.
The drawbacks of at-home sleep studies
Though the allure of at-home sleep studies is undoubtedly strong, there are some drawbacks to consider.
Limitations in data collection
While at-home sleep studies offer convenience, they may not capture as comprehensive data as those conducted in a clinical setting. Certain physiological measures can be more accurately monitored in a lab, where trained professionals can ensure proper calibration and handling of equipment.
This limitation can affect the clarity of the diagnosis, so it’s essential to weigh this when considering your options.
Potential for user error
Another concern surrounding at-home sleep studies is the potential for user error. Participants are responsible for correctly attaching sensors and ensuring everything works properly, which can sometimes lead to inaccurate data collection.
For optimal results, following the provided instructions meticulously is crucial. Even a minor error may compromise the validity of the study, which could delay receiving appropriate treatment.
Making the decision: Is an at-home sleep study right for you?
As you consider the merits and challenges of at-home sleep studies, it’s essential to reflect on your unique situation and needs.
Factors to consider
Various factors should influence your decision, including your sleep history, the severity of your symptoms, and your overall comfort with technology. If you have only mild sleep concerns, an at-home study might be perfectly sufficient. However, if you suspect a serious disorder, it may be wise to pursue a comprehensive study under professional supervision.

Consulting with a healthcare professional
Before committing to an at-home sleep study, it’s advisable to consult with a healthcare professional. They can guide you in choosing the most appropriate testing method based on your individual circumstances and medical history.
Having expert input can be invaluable in ensuring you receive the right diagnosis and treatment, ultimately helping you achieve better sleep quality and overall health.
Other resources: Sleep Study Sunshine Coast